Abstract
Introduction:
Renal insufficiency (RI) is a common feature of multiple myeloma (MM). The relative risk (RR) of disease progression or death in patients with RI was higher than those without. RI increases risk of early death and affects disease management in multiple ways in MM, as it may complicate treatment options and dosing, and render patients more susceptible to infections and prolonged hospitalizations. Therefore, there is an urgent need to figure out the most effective regimen to treat MM patients with RI. But according to our knowledge, no head-to-head trial or meta-analysis has been conducted to determine which regimen would be the best choice for those patients.
Daratumumab, an IgG1κ human monoclonal antibody that targets CD38, has shown durable responses and a favorable safety profile in both heavily pretreated patients with relapsed/refractory MM (RRMM) as monotherapy or combined with other agents and patients with newly diagnosed MM (NDMM). Pharmacokinetic analyses suggest that no clinically significant differences were found in patients with normal or impaired renal function following exposure to daratumumab, but the available data on efficacy of MM patients with RI are limited.
Thus, to generate the efficacy evidence in MM patients with RI of Daratumumab among currently available agents, we conduct this meta-analysis regarding comparative efficacy of treatments for multiple myeloma patients with renal insufficiency, and compare those of MM with RI with those of MM without RI.
Methods and methodology:
A comprehensive literature search on 3 databases (PubMed, EMBASE and Cochrane Library) was performed from inception of each database to March 30, 2022. In addition, we performed a search of the gray literature through manual hand search of conference abstracts and proceedings of the American Society of Hematology, American Society of Clinical Oncology, European Hematology Association, European Myeloma Network and European Society for Medical Oncology from 2018 to 2022.
A total of 8 studies including 4576 patients were included in this study. 2388 were in the Dara group and 2188 were in the control group. HR of OS, PFS and MRD negativity rate were computed by using a fixed-effect model by RevMan v.5.4.
Results:
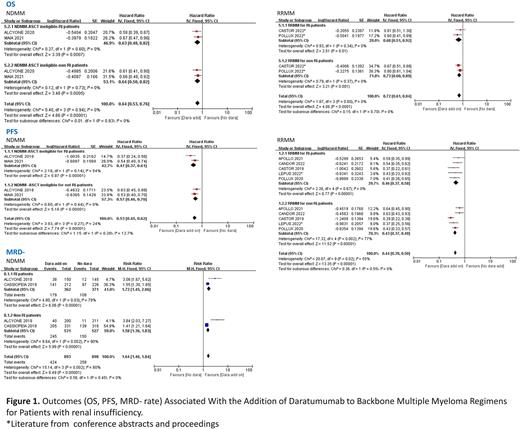
Among the included studies which conducted in the NDMM patients, MAIA and ALCYONE studies reported mature median OS data. The meta-analysis of these two studies showed the addition of Daratumumab to backbone regimens in transplant-ineligible NDMM with RI significantly improved the OS (pooled HR, 0.63; 95%CI, 0.48-0.82; P = .0007). Similarly, Daratumumab addition to backbone regimens in RRMM patients with RI decreased the risk of death (Pooled HR, 0.68; 95% CI, 0.51-0.92; P = .01).
In the meta-analysis, the addition of daratumumab to backbone regimens in NDMM among patients with RI was associated with improved PFS (pooled HR, 0.46; 95%CI, 0.36-0.57; P < .00001). Similar results were seen for RRMM patients with RI (pooled HR, 0.46; 95% CI, 0.37-0.58; P < .00001).
2 studies (Alcyone, Cassiopeia) conducted in NDMM patients had subgroup analysis of MRD- rate in MM with RI, the meta-analysis showed that the addition of Daratumumab to backbone regimens could lead to higher MRD- rate (Risk ratio, 1.72; 95% CI, 1.45-2.06; P<.00001).
Meta-analysis conducted among patients with non-RI showed that addition of Daratumumab to standard of care treatment significantly improved the OS (NDMM: pooled HR, 0.64; 95% CI, 0.50-0.82; P =.0005; RRMM: pooled HR, 0.73; 95% CI, 0.60-0.89; P = .001) and PFS (NDMM: pooled HR, 0.57, 95% CI, 0.47-0.69; P<.00001; RRMM: pooled HR, 0.43; 95% CI, 0.37-0.49; P<.00001) in both NDMM and RRMM. And MRD- rate was improved as well (NDMM: Risk ratio, 1.58; 95% CI, 1.36-1.83; P<.00001).
Through the test for outcomes of MM patients with RI and non-RI, the result showed that the addition of Daratumumab to the backbone regimens can improve the OS (NDMM: p=0.93; RRMM: p=0.70), PFS (NDMM: p=0.28; RRMM: p=0.55) and MRD- rate (NDMM: p=0.45) of MM patients with RI and non-RI in both NDMM and RRMM to the same extend.
Discussion:
This study suggests that the addition of Daratumumab to the backbone regimens can lead to longer OS, PFS and achieve higher MRD- rate among patients with RI and non-RI in the context of newly diagnosed and relapsed or refractory disease.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal